
TREATMENT AND PROGNOSIS
You will likely receive several different treatments while in hospital for a lung flare-up. It is important to understand the role of each treatment and to ask if you are unsure why it is being prescribed. Review some of the common therapies below and click on the image to find out more.
Possible treatment options

Relievers

Corticosteroids

Antibiotics

Oxygen


Non-invasive ventilation

Physical activity

Respiratory therapy

Allied health therapy
A hospital admission for a flare-up can be a good prompt to review your preventative strategies with your doctor.
Role of the healthcare team
Hospitals are dynamic places that aim to deliver the best care for people with COPD via a large multi-disciplinary team. This includes a range of medical, nursing and allied health professionals as well as people involved in patient services and administration. In order to optimise your care experience, it is helpful to have a clear understanding of the roles of some of these professionals.
Click on the boxes below to learn more about your healthcare team.

Medical Practitioners (Doctors)
Nurse
Ward or Nurse Unit Manager
Physiotherapist
Dietician
Social Worker
Occupational Therapist
Pharmacist
Psychologist
Indigenous Liaison Officer
Prognosis after flare-ups of COPD
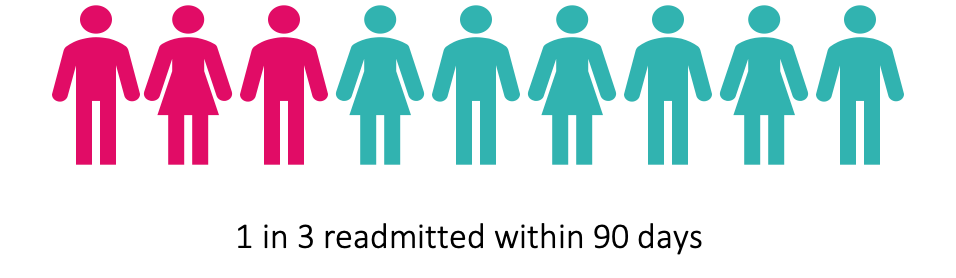
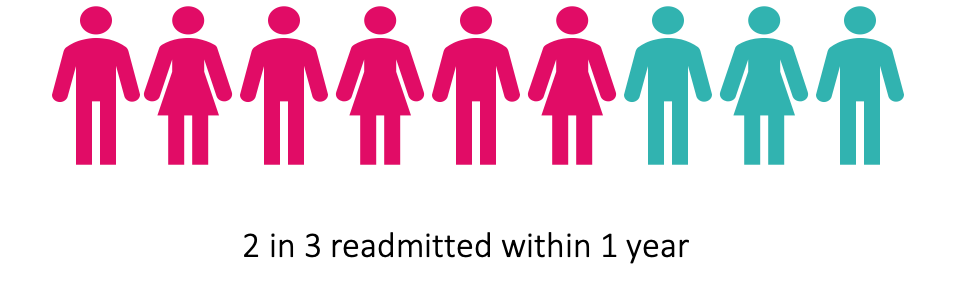
Flare-ups of COPD are serious events associated with reductions in lung function, quality of life, muscle strength and physical activity levels. Recovery can be slow or sub-optimal if no action is taken. They also increase the risk of further flare-ups, readmissions and premature death. The greatest risk for experiencing a COPD flare-up is a history of a past COPD flare-up (particularly in the last year).
Optimising recovery after a flare-up is important to reduce the risk of further flare-ups. Ensure you have a recovery plan in place before you leave hospital.
Strategies that may help to prevent flare-ups include:
- Using your COPD Action Plan developed with your GP / lung specialist.
- Familiarising yourself with your symptom pattern so you can identify early signs of becoming unwell.
- Learning about your triggers (e.g. chest infections, heart failure, exposure to tough weather and pollutants, psychosocial stressors).
- Having up-to-date immunisations for flu and pneumonia.
- Being diligent with hand hygiene and distancing from people with colds and flu.
- Taking medications consistently and correctly including correctly using your inhalers.
- Keep as physically well as possible by ensuring a healthy diet, exercise and sleep habits.
- Optimise your recovery from the last flare-up.
