EARLY MANAGEMENT
Recognising the signs of a COPD flare-up and starting early, pro-active treatment is crucial to prevent your flare-up from worsening.
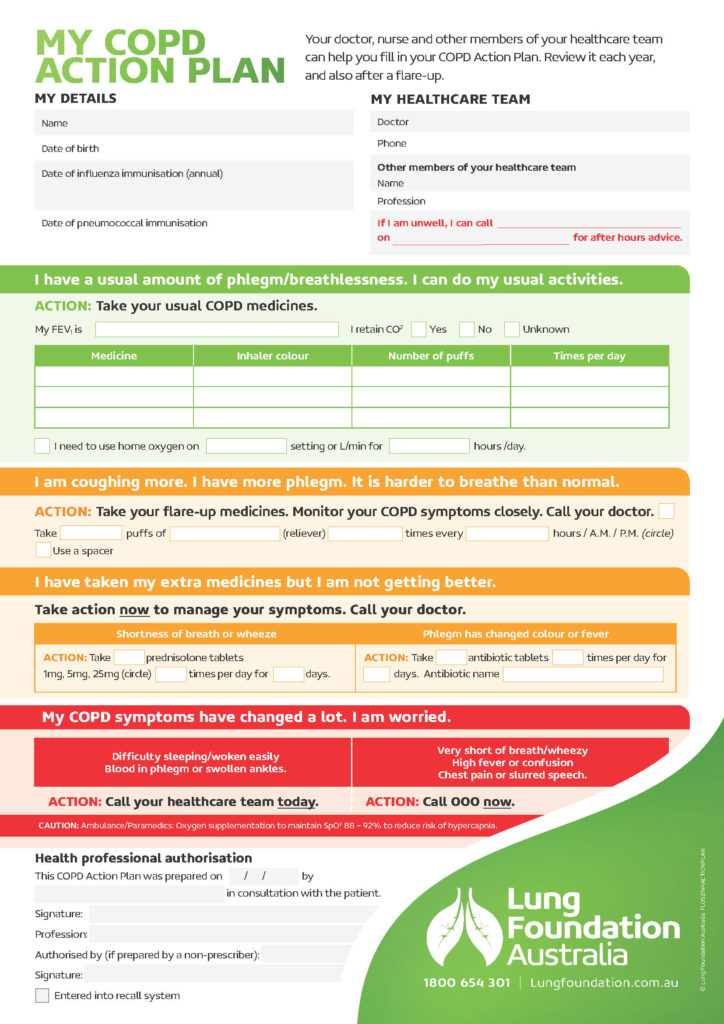
Different people may need different treatments – knowing what’s the right course of action for you is essential. This is typically set out in a COPD action plan.
Flare-up action plan
- Follow your COPD action plan that was previously discussed with your GP / lung specialist.
- Download a COPD action plan form.
- The action plan should be reviewed every six months, or after every flare-up.
- Contact your GP or lung specialist early. Do not ‘wait and see’.
- Initiate additional medications as planned.
- Pace your activity by breaking up tasks and allowing more time to complete them. Plan to be restful after a task requiring exertion.
- Use breathing techniques and comfortable resting positions to manage breathlessness. Use airway clearance techniques to clear mucus from your airways if previously taught by a physiotherapist.
- Drink and eat small amounts of nourishing foods but more frequently.
- Contact your doctor again if your flare up feels severe, or if you need to take your fast-acting relievers more often than once every 3 hours.
“I use my action plan religiously. It’s reassuring to have in writing exactly what I need to do if I have a flare-up. Listen to your lungs and know when to refer to your action plan.”
– Jan, who has COPD
Take action early: delaying initial treatment of a lung flare-up by 24 hours or more can double the risk of a hospital admission.
When to go to hospital
The following signs may indicate a need to present to hospital for rapid treatment:
- Significant increase in the intensity of symptoms;
- Severe COPD; or
- Increased symptoms alongside: Inadequate response to medical treatment in the community.
- Co-existing serious chronic health conditions.
- Inability to eat or sleep.
- Altered mental status.
- New physical signs such as bluish discolouration, swelling in limbs or a change in heart rate or rhythm of concern.
- Inability to walk between rooms when able to do so usually, or difficulty managing at home even with supports in place.
- Insufficient medical support where you are.
Call an ambulance if you are:
- Finding it hard to talk
- Finding it hard to walk
- Not able to sleep because of breathing difficulty
- Feeling drowsy or confused
- Having blue or grey discolouration of your lips or fingernails
- Having a fast or irregular heartbeat / pulse