
HEALTHY HABITS
Non-pharmacological treatments (those that do not involve drug or medication therapies) are an important part of comprehensive COPD management in conjunction with pharmacological treatments to improve symptoms, improve quality of life, slow disease progression and reduce the risk of exacerbations and premature death. Examples of important non-pharmacological management options include quitting smoking, maintaining adequate levels of physical activity and/or exercise, ensuring you adopt healthy dietary and nutrition habits, and optimising your mental and emotional health and well-being.
Smoking cessation
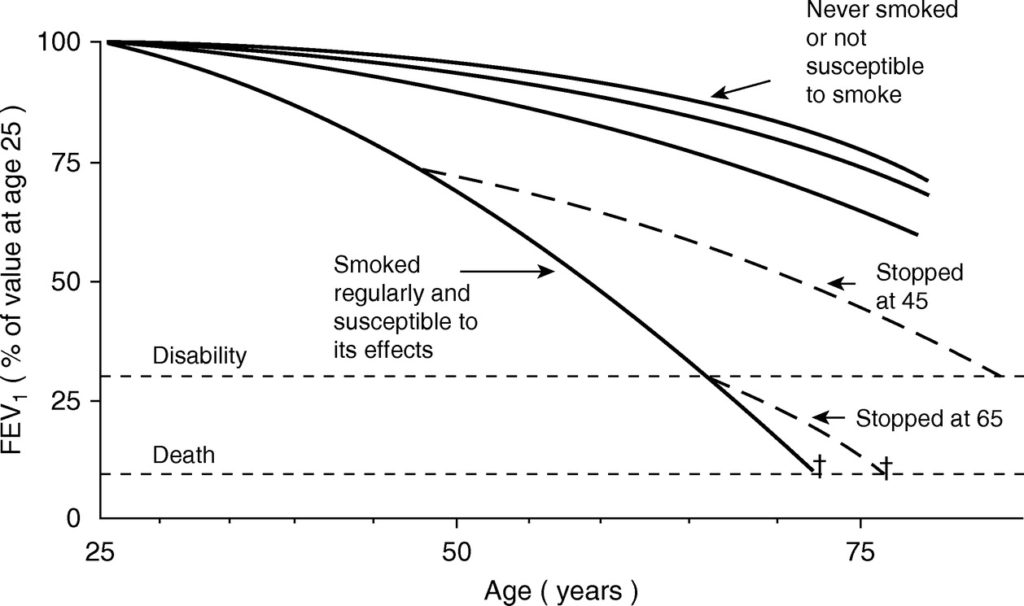
Just as smoking has been an established driver of accelerated lung function decline, smoking cessation has also been firmly proven to improve (slow) the rate of lung deterioration and delay the development of disability. Smoking is a significant modifiable factor in the treatment of COPD.
The graph below shows a set of curves that demonstrate the rate of lung function decline and risk of death and disability for men who do and do not smoke, with smoking causing a faster worsening of these outcomes.
Furthermore, smoking cessation reduces your risk of lung cancer, and heart and circulation disease. Avoiding exposure to other irritants such as fumes and pollutants is also key to preventing accelerated disease progression.
Stopping smoking is a process rather than an isolated event for most people, and is not simply ‘stopping a bad habit’. Nicotine addiction is a recognised medical condition, requiring a bundled approach comprising personalised cessation advice and a combination of behavioural counselling and pharmacotherapy. Learn more about overcoming challenges and getting support to quit smoking here.
Quitting smoking is the most important priority in COPD – discuss treatment options with your healthcare professional.
Physical activity & exercise
Keeping physically active through activities such as walking and/or exercise is good for your overall health and wellbeing. In COPD it is even associated with lower risk of future flare-ups and hospitalisations. Being inactive or sedentary for long periods (even if you are doing some physical activity) counteracts these benefits and should be minimised.
It can be difficult for people with COPD to keep active due to breathlessness on exertion, fatigue and/or other physical and mental health conditions. But it is essential and can improve with the right support.
Keeping active is crucial whether you have mild, moderate or severe disease.
Adequate physical activity levels across the week to achieve benefits for adults with COPD include:
At least 5 days a week of:

30 minutes of at least moderate intensity physical activity (e.g. aerobics class or dynamic sports)

Participating in everyday tasks requiring the use of muscle strength e.g. gardening or lifting

Enjoyable activities (e.g. golf, Tai Chi, bowls)
If you have completed a pulmonary rehabilitation program within the last year, there may be a specialised exercise program run by trained professionals aiming to maintain the benefits gained from pulmonary rehabilitation available to you. In Australia, Lungs in Action is a maintenance program that can accommodate oxygen devices and mobility aids. Locate a program near you or contact your local community health service to find suitable options for you.
Watch the video below by the Lung Foundation Australia about maintenance exercise programs.
Diet and nutrition
Malnutrition and obesity are commonly encountered in COPD. Malnutrition occurs because of a lack of energy intake due to breathlessness when eating, the pressure on the stomach from hyper-inflated lungs and loss of appetite as a side effect of medications. High calorie nutritional supplements should be considered for people who are malnourished or have severe disease, and it is also important that individuals undergo nutritional therapy before declaring a state of malnutrition.
Obesity at the other end complicates COPD management. Obesity is associated with increased use of inhalers, breathlessness, fatigue, and overall reduced exercise capacity and quality of life. However, obesity in COPD can lower the risk of death.
The aims of nutritional management in COPD are to eat a balanced diet with a variety of foods, and maintain a healthy weight.
Eating strategies when breathless |
|---|
| Plan to eat nutritious small meals and snacks more frequently, avoid large meals |
| Avoid drinking with meals |
| Eat slowly |
| Choose foods that are easier to chew and swallow e.g. mashed potato, banana |
| Limit foods that cause bloating e.g. cauliflower, beans, onions |
| Clear airways of mucus before eating |
| Plan to rest upright for 15-20mins after eating |
| If supplemental oxygen is used, wear it when eating |
| If underweight, use nutrient-rich foods to boost protein and calorie intake such as milk powder, cream, cheese, peanut butter, milkshakes or nutritionally complete oral supplements e.g. sustagen |
| Consider a referral to a dietitian for individual advice |
Mental and emotional well-being
It is common for people with COPD to experience negative impacts on mood and/or emotion at some stage of their disease. Poor mental health, particularly anxiety and depression, can lead to poor self-management, feelings of helplessness and social isolation. It can be hard to recognise when you may be experiencing poor mental health, but various treatment options are available if you seek help.
Caring for your mental and emotional wellbeing does not necessarily mean taking medications for anxiety or depression (although they can be important for some people). Strategies such as self-care, psychological support & therapies, pulmonary rehabilitation or simply connecting with people who can share similar experiences of COPD can help.
Self-care is not simply indulgence, but refers to a regular commitment to undertake activities identified to guard your wellbeing. These activities and benefits from undertaking them are different for each person. This template can help you identify and plan self-care activities that can be integrated into everyday life. You can also learn more about peer support or initiate practices for mindfulness and self-compassion which support your ability to self-manage your disease.