
HEALTHY HABITS
The main goals of treatment for bronchiectasis are to preserve lung function and halt disease progression, optimize well-being and quality of life, minimize the frequency of exacerbations and prevent complications. In children, this is extended to optimizing lung growth and reverse structural lung injury.
A broad guide to managing bronchiectasis when you are well is outlined in the following guide produced by the Lung Foundation Australia – Stepwise management of stable bronchiectasis.
Non-pharmacology treatment (those that do not involve drug or medication therapies) are an important part of comprehensive bronchiectasis management in conjunction with pharmacology treatments to improve symptoms, reduce flare-ups and slow progression and reduce the risk of exacerbations. Examples of important non-pharmacological management options include: airway clearance therapy, optimal hydration, maintaining adequate levels of physical activity and exercise, healthy diet and nutrition habits and prioritizing your mental and emotional health and well-being.
An outline of a step-wise approach to managing bronchiectasis is presented in Figure below.
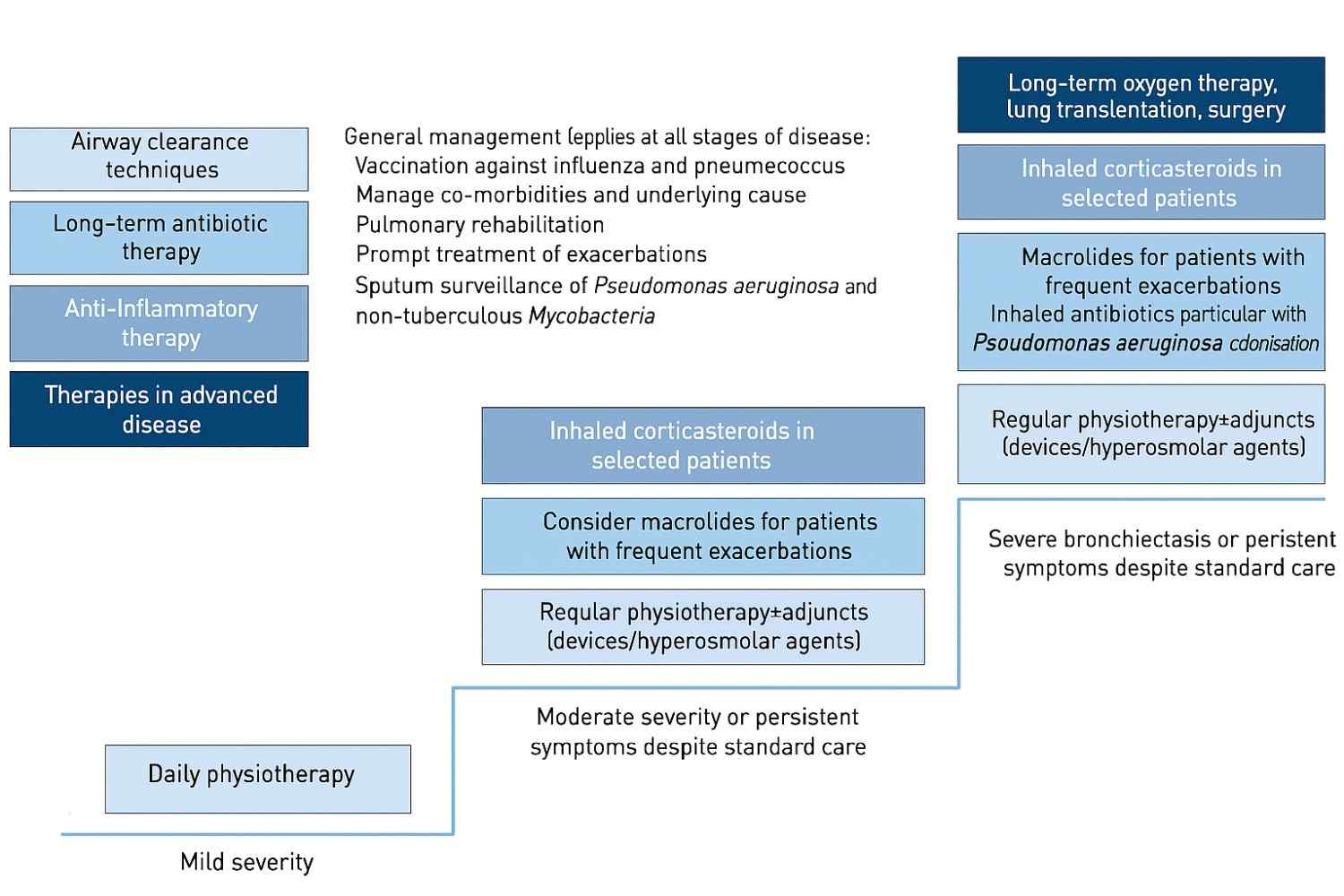
Figure : Example of a stepwise approach to bronchiectasis management
Airway clearance therapy
Clearing the excess mucus you produce on a daily basis is critical for reducing the risk of infection and acute exacerbation. Undertaking regular airway clearance therapy improves the amount of mucus you expectorate, reducing coughing and improves quality of life and can reduce the frequency of flare-ups.
Ideally, you should see a physiotherapist who has knowledge and experience in prescribing airway clearance therapy for people with respiratory conditions, including bronchiectasis. They will work with you to determine what is the best technique (or combination of techniques) for you to undertake regularly to clear your mucus. Ideally, you should have a regular review with a physiotherapist, to check your technique and made sure you are on the best program to maximise your benefit.
Doing airway clearance therapy daily is crucial to keeping well
The summary from the Lung Foundation Australia gives a further description of the importance of these airway clearance techniques
https://lungfoundation.com.au/blog/bronchiectasis-mucus-clearance-techniques
Further details of options for airway clearance therapy techniques are available on the Bronchiectasis Toolbox (www.bronchiectasis.com.au)
Hydration
Optimal hydration is necessary to enable the small cells in your lungs (cilia) to work efficiently to clear the excess mucus from your airways. If you are dehydrated due to not drinking sufficient water, infection, airline travel, altitude, air conditioning or some medications, it may be harder for you to clear your mucus. It could also increase your risk of falls, urinary tract infections and constipation.
Some key tips to assist in hydrating your airways are:
Strategies for hydration |
|---|
| Ideally breath through your nose |
| Appropriate fluid intake – drink adequate fluids (unless your fluid restriction) |
| Monitor the colour of your urine (it should be pale) |
| Limit caffeine intake |
| Sip water regularly throughout day |
Some people with bronchiectasis may require additional inhalation therapy, such as isotonic or hypertonic saline to help with the expectoration of thickened mucus. If you suspect you need this, consult with your medical practitioner and physiotherapist.
Maintaining adequate exercise and physical activity
Keeping active through a range of activities which are of interest to you is good for your overall health and may help to reduce your susceptibility to infections. Ideally, you are aiming for 5 days a week of activity for at least 30 minutes at a moderately intense pace (brisk walking, jogging, aerobic classes or dynamic sports). To help keep you motivated, it is important to choose something that you are likely to enjoy.
Some people with bronchiectasis, to get them started on their exercise routine, may undertake a pulmonary rehabilitation program, which is a structured program run by healthcare professionals (physiotherapists or exercise physiologists), who will prescribe a suitable exercise program for you. This will last for a duration of 8 weeks for most programs and you will be set up with an ongoing exercise program or routine at the conclusion. Should you need to know more about pulmonary rehabilitation, select the following link: https://lungflarecare.com/bronchiectasis-home/recovery-after-bronchiectasis/pulmonary-rehabilitation/
If you need some guidance for locating a pulmonary rehabilitation program, select this option: https://lungfoundation.com.au/patients-carers/support-services/lung-disease-and-exercise/pulmonary-rehabilitation/
Diet and nutrition
Malnutrition and being underweight are commonly encountered in bronchiectasis. Malnutrition occurs because of the lack of energy intake due to the chronic inflammation and at times infections in the lungs. Appetite can also be diminished as a side effect from some medications. If you are underweight, high calorie nutritional supplements should be considered.
Mental and emotional well-being
It is common for people with bronchiectasis to experience a low mood or negative emotions or anxiety at some stage of their disease. Anxiety and depression can both contribute to poor self-management and social isolation.
A range of strategies are available which may be helpful. While these include medications for anxiety and depression, this can be coupled with self-care options, psychological support and counselling or sharing your experience with a group of peers who have a similar diagnosis.
This template (link: https://lungfoundation.com.au/resources/self-care-template/) can help you identify and plan self-care activities that can be integrated into everyday life.
In addition to this, the Bronchiectasis checklist will help to keep track of what is in your healthcare plan to manage your condition. Select this link for a copy of the Bronchiectasis Checklist and a stepwise management guide to review when your condition is stable.