DIAGNOSING BRONCHIECTASIS
Bronchiectasis is diagnosed using a high-resolution computed tomography (HRCT) scan of the chest, a sensitive and specific imaging technique. This provides detail of the lung tissue and airways and indicates the severity of the condition. The most important finding from a CT scan is the bronchial dilatation. The dilatation is defined as the internal bronchial diameter being greater than that of the adjacent pulmonary artery. This is called the signet-ring sign (Figure below)
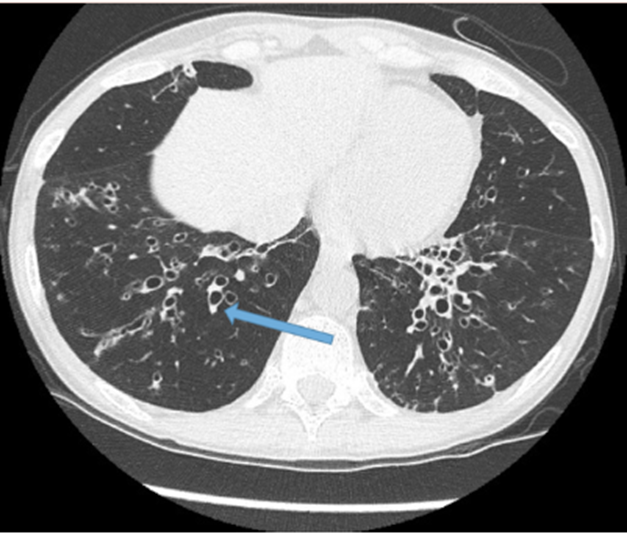
The figure above: Elderly male patient with COPD and bronchiectasis. Arrow pointing to signet ring sign
An HRCT should be considered for an individual who has the clinical phenotype of bronchiectasis, which includes chronic cough, sputum production and recurrent exacerbations (or flare-ups) to confirm a diagnosis. In addition, further information may be gathered, from the following details:

History (frequency and impact of exacerbations) and exploration of potential causes

History of exposure to tobacco smoke, cigarettes and vaping

Immunization and early childhood medical and social history
Other tests which may be ordered by your doctor may include:
- Blood tests
- Sputum tests (identify the presence of certain bugs in the mucus)
- Chest x-ray
A blood test may be done to check the levels of inflammatory markers in the blood, which may be elevated in the presence of an acute exacerbation (flare-up) or may be used for the purpose of establishing the underlying cause.
A sample of sputum will be collected to enable testing for specific bugs/germs in the mucus and guide the presence of infection. Purulent or mucopurulent mucus is frequently indicative of an infection or colonization with a chronic germ. Common bugs which may be present in mucus of people with bronchiectasis are: Haemophilus influenzae, Pseudomonas aeruginosa, Streptococcus pneumoniae, Staphylococcus aureus, Aspergillus fumigatus. The presence of these bugs will direct the necessary medical therapy (antibiotics and anti-inflammatories).
A chest x-ray may be used once a diagnosis has been established, particularly if an acute exacerbation (flare-up) is present. This may show signs of mucus plugging, consolidation or areas of lung collapse
A summary fact sheet for bronchiectasis is available from Lung Foundation Australia.